Please note that every patient and clinical situation is different, requiring prudent evaluation and decision-making by the clinician.
Each clinician is ultimately responsible to prepare and educate themselves using a variety of sources.
The following are general opinions and suggestions based on individual experiences.
Bone Allografts
Where does graft come from? Are there different types?
- Allograft – from a donor of the same species (human)
- Xenograft – from a donor of a different species (bovine, porcine, equine)
- Autograft – from the patient’s own body
- Alloplast – synthetic material
Demineralized vs Mineralized Allografts
- Mineralized – these materials retain the minerals from the tissue donor. With minerals still in tact, these grafts can heal, stabilize, and turnover to host-bone rather quickly
- Demineralized – during manufacturing, the donor minerals are removed. Theoretically, this exposes BMPs (bone morphogenetic proteins), which can serve as precursors to osteoblastic (bone building) activity. Research is somewhat inconclusive regarding BMP bioavailability and clinical significance. Many clinicians use demineralized grafts for ectopic ridge augmentations or sinus lifts. These materials, however, typically don’t heal and turnover to host-bone as quickly as Mineralized.
Cancellous vs Cortical Allografts
- Cancellous – made from donor cancellous, spongy, or trabecular bone. These grafts are very porous and allow extensive blood infiltration. These grafts promote quick, stable clot formation, which yields excellent results, especially in socket grafting procedures
- Cortical – made from donor compact, or cortical bone. These grafts are dense and strong. Cortical grafts resorb and turnover slowly, which can be beneficial for large graft sites, or where space maintenance is especially crucial. Many clinicians use cortical grafts for sinus lifts or ridge augmentations.
- Cortical/Cancellous Mix – many clinicians find these to be the best of both worlds
How much graft do I need?
- .25cc is typically enough for a central incisor socket graft
- .5cc is typically enough for an anterior socket graft
- 1cc is typically enough for a large premolar, or molar socket graft
- 2cc is typically used for multiple adjacent socket grafts, sinus lifts, or other large graft areas
**To maintain sterility and patient safety, we don’t recommend the use of grafts in volumes larger than 2cc**
Can I use one jar of graft in multiple procedures or patients?
- Simply put…No. Bone grafts and other regenerative materials are single-use only, and must be used on ONE patient in ONE appointment. Ignoring this protocol may subject your patients to cross-contamination.
If I don’t use an entire jar of graft during my procedure, what do I do with the remainder?
- Tissue can be safely disposed-of with the other biologic waste in your practice
Do I need to hydrate the graft before placement?
Yes! Our grafts are conveniently packaged inside jars that can be used as dappen dishes. Grafts should be hydrated 10 minutes prior to surgical placement. Grafts can be hydrated in:
- sterile saline
- epinephrine-free anesthetic
- blood collected from the surgical site
- blood collected intravenously
- PRP/PRF
- metronidazole or other antibiotic solution
Are bone allografts safe?
The short answer is “yes, they’ve proven themselves safe.” There are always minor risks, but our donor screening, processing techniques, and sterilization protocols are better than industry standards, AATB Certified, and FDA compliant. Click here for more information.
What if the extraction site is infected?
Membranes
When do I need to use a membrane?
The short answer: nearly every time! Membranes are especially necessary when primary closure IS NOT achieved, because the membrane will help protect and contain the graft material in the socket/defect/augmentation site. Even when primary closure IS achieved, the membrane serves to inhibit soft tissue from growing INTO the bone graft material. If soft tissue ingrowth occurs, the bone graft won’t heal properly, or turnover into bone optimally.
What type of membrane should I use?
There’s a lot that goes into this decision, so these are just general thoughts and recommendations.
Non-resorable – When primary closure is not achieved. Resorbable membranes, even those that are long-lasting, can’t survive the oral environment as long or as predictably as needed. A PTFE membrane is best in this situation.
Resorbable – When primary closure is achieved. The membrane will serve to inhibit soft tissue ingrowth into the bone graft material. Collagen membranes are an excellent choice, as well as pericardium.
How long should I leave the membrane in place after surgery?
Generally, most clinicians leave non-resorbable membranes in place for 3-5 weeks. You should see the patient a number of times during this period so you can evaluate when the tissue is ready for membrane removal.
Can I use one membrane in multiple procedures or patients?
- Simply put…No. Membranes and other regenerative materials are single-use only, and must be used on ONE patient in ONE appointment. Ignoring this protocol may subject your patients to cross-contamination.
If I don’t use an entire membrane during my procedure, what do I do with the remainder?
- Tissue can be safely disposed-of with the other biologic waste in your practice
Sutures
What suture size should I use?
3-0 Large diameter thread. These can be used in full-arch cases, or where strength is the ultimate need
4-0 or 5-0 These are your go-to, all-purpose thread sizes
6-0 Microsurgery, or other presentations of delicate tissue. This includes very thin tissue, or delicate papillae
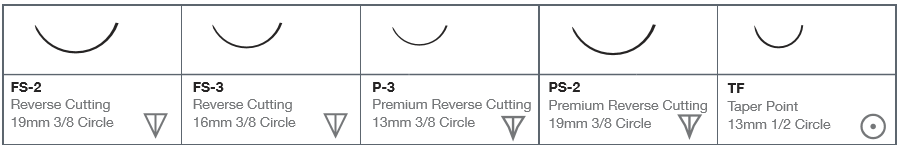
What needle types are there and how do I know which to use?
Instruments
What do I need to get started in socket preservation?
We recommend starting with the basics for atraumatic extraction. It’s always easier to preserve tissue than regenerate it. This includes:
- blade holder
- Castroviejo needle holder (NOT hemostats)
- elevators
- periosteal elevators
- periotomes (flexible is preferred)
- spoon curettes
- serrated curettes
- root-tip extractors
- tissue forceps
- corn-suture forceps
- forceps
- retractors
- mouth props
- surgical piezo (for the highest level of efficiency, and to ensure the most conservative and safe treatment)
Our team of clinicians have curated two kits that contain the best combination of easy-to-use and efficient instruments. Click here to see more.
What do I need to be able to do sinus grafts?
In addition to the above, you’ll need:
- concave osteotomes/mallet for vertical-approach augmentations
- specialty hand instruments for releasing/preserving the Schneiderian membrane
- zirconia-tipped burs for lateral-approach augmentations

